Thanks to steroids

Thanks to steroids Mia's lupus is quiet right now

Thanks to steroids Mia's lupus is quiet right now
But her side effects are raging
Steroid-toxicity has been hiding in plain sight for over 75 years — enough is enough
1948
First clinical use of cortisone, a glucocorticoid.
23 days later
First report of toxicity and The Great Taper began.
2016
Glucocorticoid Toxicity Index (GTI) first introduced.
The first synthetic glucocorticoid was developed and administered for the treatment of rheumatoid arthritis in 1948. That medical breakthrough marked an era of such significance that inventors Philip Hench, Edward Kendall and Tadeus Reichstein were awarded the Nobel Prize in Medicine in 1950.
However, just 23 days after the first dose of cortisone, the first toxicities of this new compound were reported. The very next day, the first steroid taper began, and the quest to develop steroid-sparing alternatives has continued ever since.
Recognizing the urgent need to research, monitor and reduce the use of steroids in patients and populations, a team of experts from around the world convened in 2016 to lay the foundations for development of the Glucocorticoid Toxicity Index. The GTI is the first validated clinical outcome assessment to measure steroid-toxicity.
Steritas was founded in 2021 to license the GTI for use worldwide, and to support all investigators who integrate the GTI into their research. In 2023, we researched and validated a collection of innovative clinical outcome assessments (COAs) of steroid-toxicity. The STOX® Suite includes solutions for adult, pediatric and point-of-care assessments.
The Great Taper®: turning the tide on steroid-toxicity
Within days of the first use of cortisone in 1948, doctors recognized the need to find the lowest therapeutic dose to manage disease and eliminate steroid toxicity. Over the next 75 years, progress in tapering glucocorticoid use was slow, due largely to the lack of: effective alternatives, consensus among practitioners on what to measure, and technology to make measurement practical, if even possible.
To confront this problem head on, Steritas launched The Great Taper® — a public initiative to accelerate a shift in steroid prescribing patterns worldwide.
In service of this movement, we built:
- The STOX Suite to measure steroid-toxicity
- The STOX Digital Platform to validate results
- Steroids and Me (Sam) to strengthen the doctor-patient connection
The Great Taper® initiative provides medical information and an online portal for patients, medical, and paramedical providers; publications and programs for the measurement and prevention of steroid-toxicity; and curated, professional, expert content regarding the public health issue of steroid-toxicity.
This body of work establishes an essential framework to step up The Great Taper® and put the burdens of steroid-toxicity behind us for good.
Altering steroid prescribing patterns for good
In our mission to alleviate the heavy burdens of steroid-toxicity, Steritas established the STOX Suite, a selection of world-class clinical outcome assessment (COA) tools for measuring steroid-toxicity.
We collaborate across all subspecialties to provide the most effective solutions for use in:
- Clinical research for development of new steroid-sparing drugs and treatment protocols
- Health and economics outcomes research (HEOR) for discovery of steroid-toxicity and hidden costs found in large datasets
- Routine practice to monitor emerging steroid-toxicity in clinic patients
- Direct-to-patient applications that help patients collaborate in their treatment
The Steritas STOX Suite (GTI, GTI-MD, and pGTI) has been used in over 75+ clinical trials, in 1100 sites across 80 countries.
Steroid Side-effects
Over 80 steroid-toxicities are on record, ranging from inconvenient to life-threatening. In pediatric illnesses, steroids are especially cruel and persist into adulthood – affecting growth and disrupting the psychosocial development of our children.
To learn more about the range of side effects, watch the video.
"The complications and risks of long-term steroids are real in the lives of many. They are challenging, they are expensive, and they are lasting."
John, a patient in his 60's
"I went from being a strong, confident leader to someone who cried most of day, couldn’t sleep, and was extremely agitated. I spent the next six years going through the roller coaster of flares and remission. With each steroid taper I felt like I was going through drug withdrawal. I’ll do just about anything to avoid the swings that come along side with them."
Kathy, a patient in her 60's
"I’m a new grandfather. I would love nothing more than to get on floor and play with my grandkids. What I hope for most of all is an improved quality of life to deal with vasculitis and also deal with the side effects of prednisone."
Glen, a patient in his mid 60s
"The combination of chemo and steroids is a very tough treatment to go through. I did not recognize the person that I had changed into. My biggest struggle was feeling like I couldn’t be the mother that I previously was to my children."
Trina, a patient in her 40's
The true cost of steroids
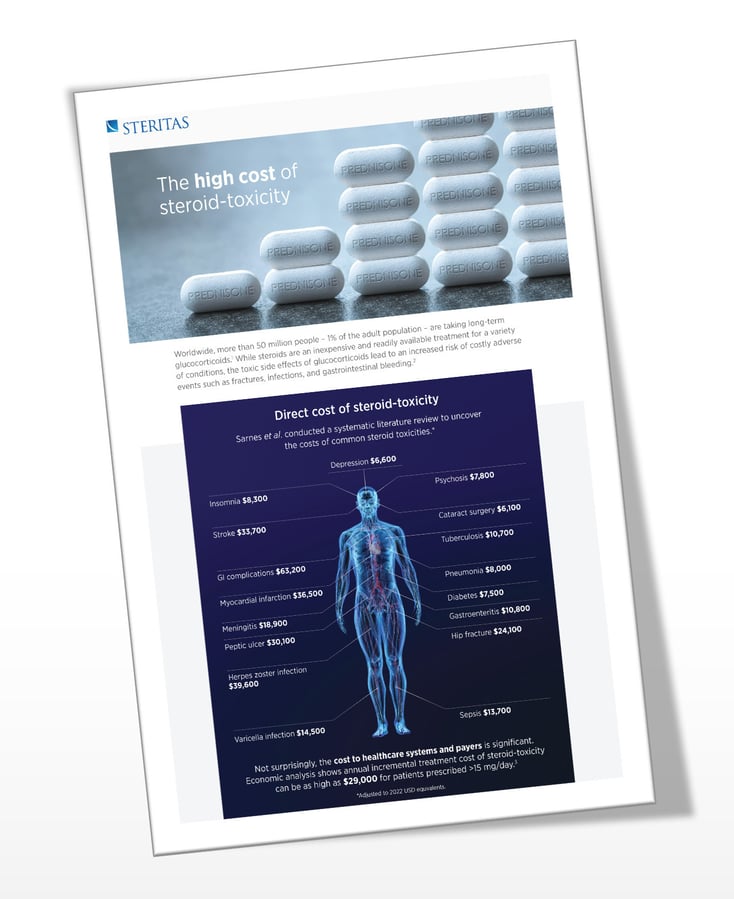
At first glance, steroids appear less costly than other inflammatory disease medications, but research continues to reveal that the true economic impact of steroid use is staggering.
A study revealed that the adverse effects of glucocorticoids accounted for 40% of medical costs for patients taking glucocorticoids in high doses or for longer than 60 days, for a range of autoimmune and inflammatory diseases. Strikingly, only 25% of their medical costs were disease related.[1]
A second study of systemic lupus erythematosus patients reported that high-dose glucocorticoid users were 30% more likely to have emergency room visits, 80% more likely to be hospitalized, and incurred about three times greater average annual total healthcare costs as compared to low-dose glucocorticoid users.[2]
A third longitudinal study of severe asthma demonstrates that steroid-toxicity at year one predicts steroid-toxicity at year three, even in the face of reduced exposure to steroids. These findings suggest that alternatives are introduced too late.[3]
The STOX Suite is at the center of all efforts to:
- Quantify the impact of steroid-toxicity on patients
- Make evidence-based calculations of the burden on populations
- Validate results to reduce healthcare costs
More work is underway in economic disutility, fiscal modeling and societal fiscal value of steroids and steroid alternatives. We expect the STOX Suite to be a pivotal component of the most rigorous analysis in these areas.
The true cost of steroids
At first glance, steroids appear less costly than other inflammatory disease medications, but research continues to reveal that the true economic impact of steroid use is staggering.
A study revealed that the adverse effects of glucocorticoids accounted for 40% of medical costs for patients taking glucocorticoids in high doses or for longer than 60 days, for a range of autoimmune and inflammatory diseases. Strikingly, only 25% of their medical costs were disease related.[1]
A second study of systemic lupus erythematosus patients reported that high-dose glucocorticoid users were 30% more likely to have emergency room visits, 80% more likely to be hospitalized, and incurred about three times greater average annual total healthcare costs as compared to low-dose glucocorticoid users.[2]
A third longitudinal study of severe asthma demonstrates that steroid-toxicity at year one predicts steroid-toxicity at year three, even in the face of reduced exposure to steroids. These findings suggest that alternatives are introduced too late.[3]
The STOX Suite is at the center of all efforts to:
- Quantify the impact of steroid-toxicity on patients
- Make evidence-based calculations of the burden on populations
- Validate results to reduce healthcare costs
More work is underway in economic disutility, fiscal modeling and societal fiscal value of steroids and steroid alternatives. We expect the STOX Suite to be a pivotal component of the most rigorous analysis in these areas.

“Tracking steroid-toxicity is critically important to improving the standard of care and reducing healthcare burden.”
John H. Stone, MD MPH
References
- Rice JB, White AG, Johnson M, Wagh A, Qin Y, Bartels-Peculis L, Ciepielewska G, Nelson WW. Healthcare resource use and cost associated with varying dosages of extended corticosteroid exposure in a US population, Journal of Medical Economics, 21:9, 846-852, DOI:10.1080/13696998.2018.1474750.
- Kabadi S, Yeaw J, Bacani AK, Tafesse E, Bos K, Karkare S, DeKoven M, Vina ER. Healthcare resource utilization and costs associated with long-term corticosteroid exposure in patients with systemic lupus erythematosus. Lupus. 2018 Oct;27(11):1799-1809. doi: 10.1177/0961203318790675. Epub 2018 Aug 1. PMID: 30068254; PMCID: PMC6264911.
- Pamela Jane McDowell, John Busby, John Stone, Kirsty Honeyford, Louise Dunn, Claire Butler, Liam Heaney European Respiratory Journal 2023 62: OA1528; DOI: 10.1183/13993003.congress-2023.OA1528