More than 6.8 million people suffer with inflammatory bowel disease (IBD), many of whom are at risk of increased morbidity due to an overreliance on steroids as a main pillar of treatment.[1]
Inflammatory bowel disease is a chronic progressive disease affecting the gastrointestinal tract with two main forms: ulcerative colitis and Crohn’s disease. Ulcerative colitis causes inflammation and ulcers in the large intestine and rectum, while Crohn’s disease affects any portion of the GI tract. Inflammatory bowel disease is characterized by periods of active disease with symptoms that include abdominal pain, bloody stools, diarrhea and weight loss. These “flares” in disease activity are interspersed by periods of remission, with few or no symptoms.
The global burden of IBD has increased over the last 3 decades
The global incidence of IBD is rising year over year, driven by improved awareness and diagnostics combined with a trend towards a more Westernized lifestyle in developing countries. Age-standardized prevalence rose from 79.5 per 100,000 population in 1990 to 84.3 per 100,000 in 2017, accounting for a total of 6.8 million IBD cases globally by 2017.[1]
This increase was balanced by an improvement in outcomes for IBD patients. The introduction of new treatments has been associated with a decline in age-standardized death rates from 0.61 per 100,000 to 0.51 per 100,000 over the same period.[1]
Chronic steroid use is an overlooked issue in IBD
The effectiveness of steroids in inducing remission in IBD has been recognized since the 1950s, and they are still widely used for this purpose in IBD treatment today. These agents are associated with a plethora of side-effects including insomnia, weight gain, hyperglycemia, hypertension, cataracts and loss of bone strength. Notably, prolonged use of steroids in IBD increases the risk of both morbidity and mortality when compared to the use of biologic and immunomodulator therapies.[2] Consequently, there are widespread initiatives to reduce chronic steroid use, with IBD guidelines in the US, UK and Europe recommending rapid initiation of tapering after induction of remission.
The impact of glucocorticoids on patient morbidity and mortality in IBD
Despite these efforts, a recent retrospective study found that the long-term use of glucocorticoids in IBD is still having a major impact on the quality of life of patients living with IBD. Farraj et. al.[4] carried out a retrospective review of data from the fourth quarter of 2015 through 2019, a database of inpatient healthcare cost and utilization from over 40 states in the US.
The study compared patients receiving chronic glucocorticoid therapy (defined as greater than 3 months of treatment) and those with a history of steroid therapy with patients who had neither chronic therapy nor a history of steroid use. A total of 283,970 IBD patients were included in the analysis, which identified 18,030 (6.4%) patients with chronic steroid use or a personal history of systemic steroid therapy.
The steroid group had significantly higher odds of morbidity, including:
- 1.9x risk of developing osteoporosis
- 2.1x increase in opportunistic infections
- 1.5x the risk of developing acute thrombotic events
- 10x increase in the incidence of Cushing’s syndrome
- 9x increased risk of developing adrenal insufficiency
These figures are consistent with the findings of a 2022 study published by researchers from the University of Gothenburg, Sweden[3], which looked at the impact of long-term steroid use across a cross-section of the population.
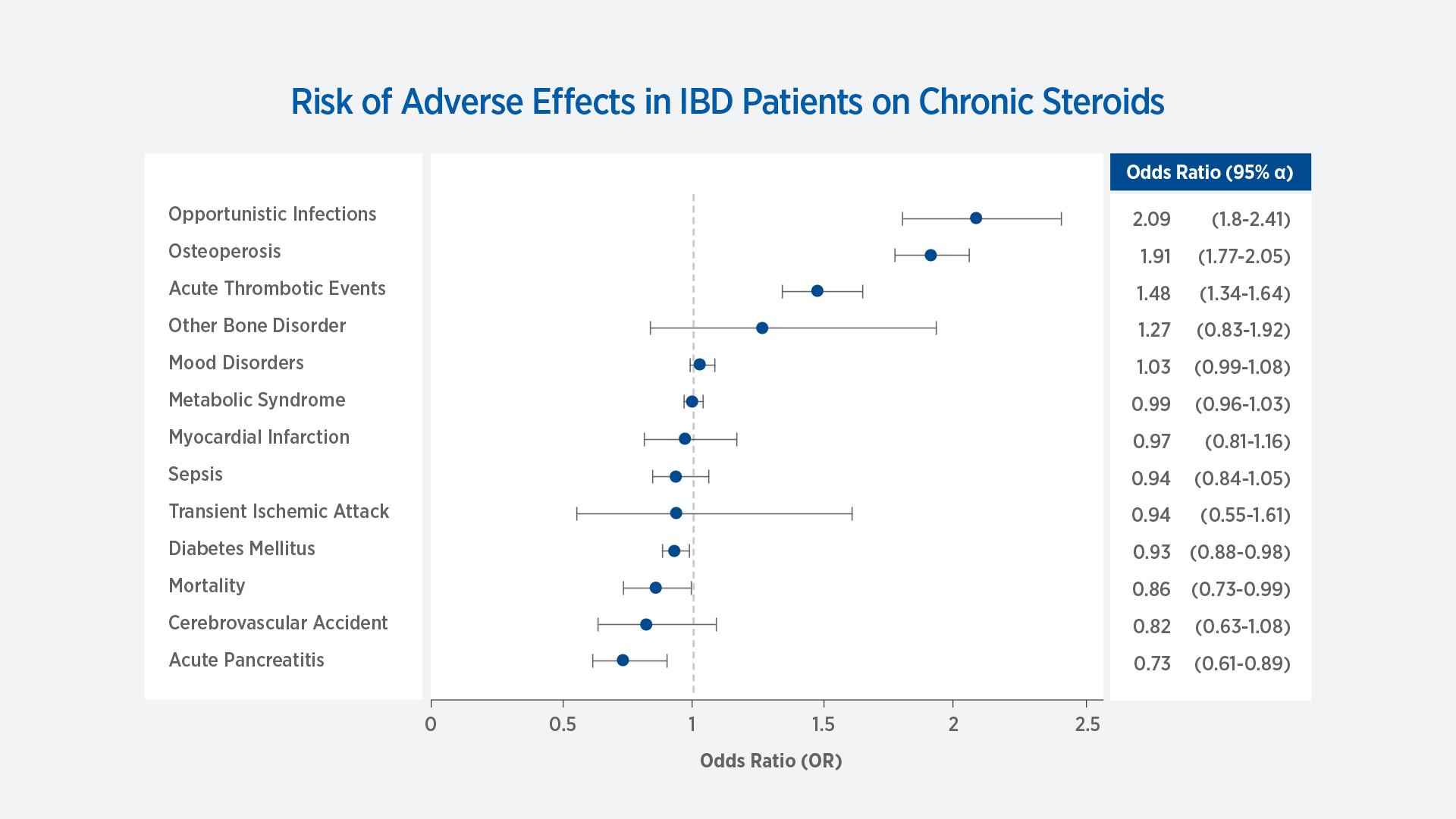
Figure 1 adapted from Farraj et al. 2022[4] Adjusted odd ratio of various adverse events in patients with inflammatory bowel disease and concurrent chronic glucocorticoid therapy compared with those not on chronic glucocorticoid therapy.
There were no significant differences between the glucocorticoid and non-steroid group in the following side effects: sepsis, transient ischemic attack, cerebrovascular accident, myocardial infarction, bone disorders or other metabolic syndrome related disorders.
Immense risk of chronic steroid use in IBD
Overall, the paper highlights the impact that chronic glucocorticoid use has on the quality of life of IBD patients, despite the best efforts of clinicians to follow steroid-sparing guidelines in favor of rapid taper and transition to other agents.
The take-home message from the authors was that prolonged use of glucocorticoids in IBD patients poses an immense risk of increased morbidity when compared to the use of immunomodulators and biological therapies.
Lea Ann Chen, MD, Director of IBD Translational Research at Rutgers Robert Wood Johnson Medical School, provided further insight into the impact of steroid-toxicity in IBD patients.
“With the recent increase of medications approved to treat ulcerative colitis and Crohn’s disease, patients now have several options for therapies they can use for IBD and limit their steroid exposure. While steroids can still play a critical role in dampening disease activity urgently and in providing symptom relief when transitioning to definitive IBD therapy, we, unfortunately, see patients who are treated for far too long or far too frequently with these medications.”
References
- GBD 2017 Inflammatory Bowel Disease Collaborators. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet, Gastroenterology & Hepatology. 5 (1): 17-30 (2019) https://doi.org/10.1016/S2468-1253(19)30333-4
- Lichtenstein GR, Feagan BG, Cohen Rd et al. Serious infection and mortality in patients with Crohn’s disease: more than 5 years of follow up in the TREATTM registry. Am. J. Gastroenterol. 107:1409-1422. (2012). https://doi.org/10.1038/ajg.2012.218
- Einarsdottir MJ, Ekman P, Molin M, Trimpou P, Olsson DS, Johannsson G, Ragnarsson O. High Mortality Rate in Oral Glucocorticoid Users: A Population-Based Matched Cohort Study. Front Endocrinol (Lausanne). 2022 Jul 8;13:918356. https://doi.org/10.3389/fendo.2022.918356. PMID: 35872995; PMCID: PMC9304700.
- Farraj KL, Pellegrini JR, Munshi RF, Russe-Russe J, Kaliounji A, Tiwana MS, Srivastava P and Subramani K. Chronic steroid use: An overlooked impact on patients with inflammatory bowel disease. J Gastro. & Hepatol. 6:910-914. (2022). https://doi.org/10.1002/jgh3.12841
